Spinal Cord Injury: What the Patient Needs to Know
Overview
Spinal cord injury is damage to the spinal cord leading to temporary or permanent functional changes such as weakness and/or numbness in the limbs. Depending on the severity of injury, symptoms can include total or partial loss of motor and/or sensory functions below the level of the injury, loss of bowel or bladder function, and impaired breathing.
Unfortunately, there is currently no treatment to fix a damaged spinal cord. Recovery is a long-term process that will involve an interdisciplinary team of health professionals and rehabilitation to regain mobility and muscle strength. Most recovery will occur within the first 6 months to 1 year following injury.
What Is Spinal Cord Injury?
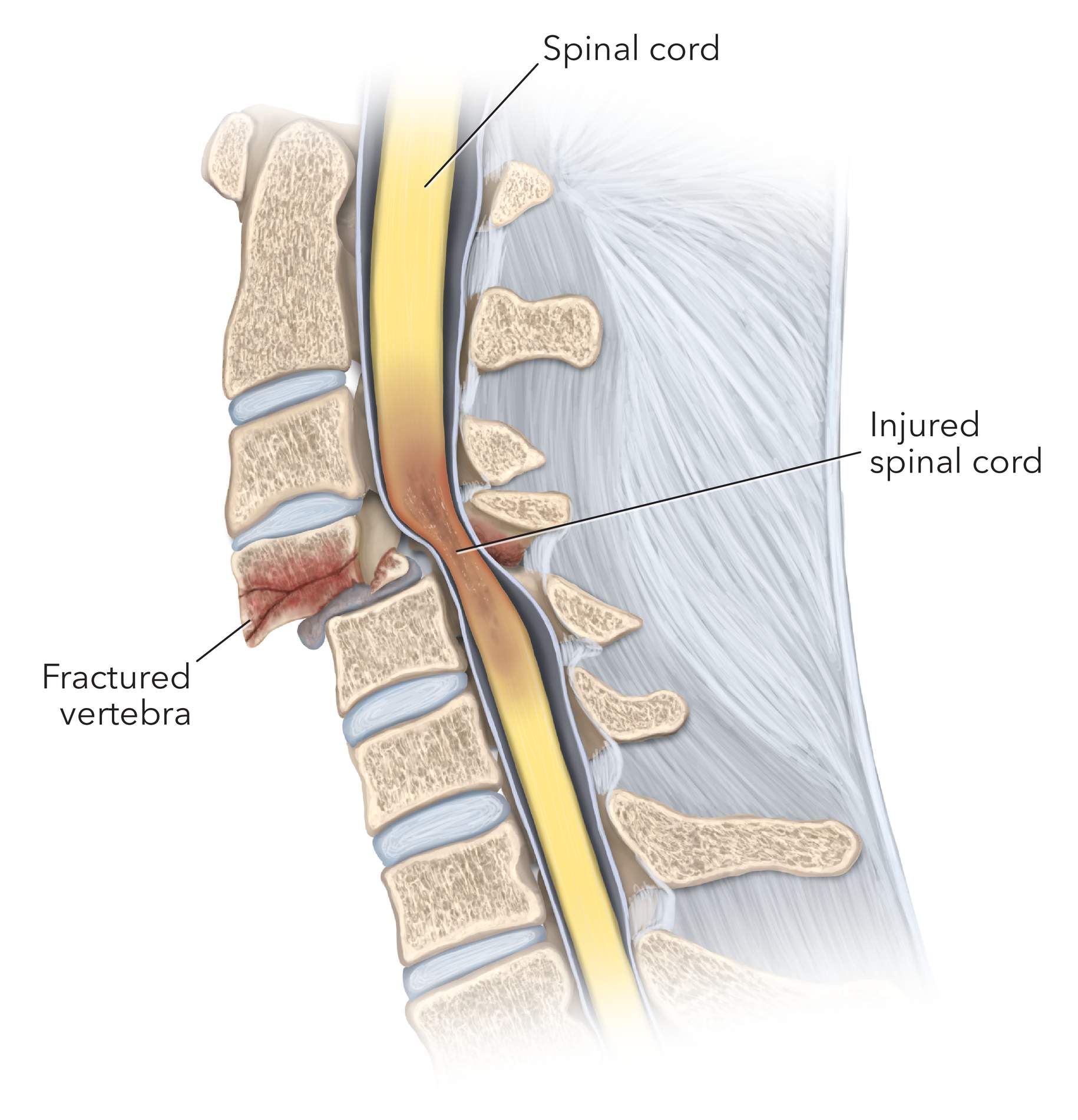
Spinal cord injury is damage to the spinal cord leading to temporary or permanent functional changes. Injury can occur through an external traumatic force such as a spine fracture or any other disease process. In traumatic spinal cord injury, damage occurs due to abrupt mechanical forces that can compress or cleave the cord. In non-traumatic spinal cord injuries, other conditions such as a spinal cord tumor, infection, multiple sclerosis, or degenerative disc can damage the cord.
The spinal cord is a long band of neural tissue housed within the bony vertebral canal. If we think about the spinal cord as an information “highway” between your brain and body, any interruption can cause loss of our ability to correctly interpret our surroundings and move the way we/our brains want to.
Approximately 50% of spinal cord injuries are unfortunately complete, causing total loss of sensation and motor functions below the level of injury on both sides of the body. The other 50% of spinal cord injuries are incomplete, causing partial loss of sensation and motor functions that may affect one side of the body more than the other.
What Are the Symptoms?
The symptoms of spinal cord injury depend on the level of the injury and the extent of spinal cord affected. In complete spinal cord injuries, patients experience total sensory and motor function loss at the level of injury and below. If the injury is incomplete, some sensation and motor function may still be present. Severe spinal cord injuries at higher levels closer to the brain (for example, at the neck) tend to affect more body parts than severe spinal cord injuries at lower spine levels.
Symptoms can include:
- Extreme pain or pressure at the site of injury
- Muscle weakness and/or loss of voluntary muscle movement
- Loss of feeling in the limbs or chest
- Loss of bladder and bowel functions
- Impaired breathing
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,000+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
What Are the Causes?
Spinal cord injuries are commonly caused by motor vehicle accidents, violence (for example, gunshot or stab wounds), sports-related injuries, and falls. In traumatic cases, injury to the spinal cord can happen due to displacement of bone fragments, damage to blood vessels which can lead to loss of sufficient oxygen supply, and disruption of neural tissues.
Other causes include infections, tumors, or degenerative processes that can gradually compress the spinal cord. Inflammatory conditions such as multiple sclerosis, toxins, and clots in the blood vessels supplying oxygen and nutrients to the spinal cord can also cause injury.
How Common Is It?
Spinal cord injury is estimated to occur in 30 – 80 people per million per year in the United States. Globally, 250,000 – 500,000 people suffer from a spinal cord injury every year. It is more commonly seen in men and young adults 30 – 40 years of age. Most injuries occur at the neck (cervical) levels.
How Is It Diagnosed?
A thorough history, mental status and neurological exam will be performed to localize the injury and determine the severity. Severity of injury is often conveyed through the 5-level American Spinal Injury Association (ASIA) impairment scale as described below:
- Grade A: Complete; No sensory or motor function preserved in the sacral segments S4 – S5 (near the tailbone)
- Grade B: Incomplete; Sensory but no motor function preserved below the neurological level and extending through the sacral segment S4 – S5
- Grade C: Incomplete; Motor function preserved below the neurological level; Most key muscles have a grade < 3 (cannot raise muscles against gravity)
- Grade D: Incomplete; Motor function preserved below the neurological level; Most key muscles have a grade > 3 (can raise muscles against gravity)
- Grade E: Normal motor and sensory function
Spinal cord injury is diagnosed through X-rays, computed tomography (CT), and magnetic resonance imaging (MRI). CT is quicker to obtain and provides better imaging of bony structures than MRI. However, MRI yields better detail of soft tissue structures of the spinal cord. CT or X-rays may be rapidly obtained during an acute setting, with MRI being performed after the patient has stabilized.
What Are the Treatment Options?
An acute spinal cord injury requires emergency medical attention. The head and neck will be immobilized to prevent movement that may cause further damage to the cord. Unfortunately, there is currently no treatment to repair a bruised or damaged spinal cord. Patients may be transferred to the neurocritical intensive care unit (ICU) for monitoring and stabilization before further supportive and rehabilitation options are discussed.
At the ICU, machines and other equipment may be used to take over functions such as urination, eating, and breathing, until the patient is able to perform these functions independently. This may be overwhelming and scary, especially after a serious accident. Some commonly used equipment include:
- Mechanical ventilator to pump oxygen into the body and perform breathing functions. This will require the placement of an endotracheal tube through the patient’s nose or mouth which will be guided downwards into the windpipe (trachea).
- Feeding tube to provide nutrition and calories if the patient is unable to feed themselves. Nasogastric tubes are inserted into the nose and down through the throat. The cap on the top of the tube can be opened to administer food and fluids.
- Bladder catheter to drain urine into a collection bag.
Surgery may be performed to emergently remove bone or disk fragments and foreign objects, or to fuse the spinal bones together and stabilize proper alignment for the bony spine.
Research is actively being conducted to discover new treatment options to regenerate nerve cells, replace damaged nerve cells, stimulate nerve cell regrowth, and retrain neural circuits. Physical therapy will be critical to gradually recovering muscle strength, mobility, communication, bowel and bladder control, and other functions. Rehabilitation will also help to prevent complications of spinal cord injury such as skin wounds, prolonged muscle contractions (spasticity), and skeletal or postural deformities.
What Is the Recovery Outlook?
Recovery from a spinal cord injury is a long-term process that will require rehabilitation and an interdisciplinary team of physicians, nurses, specialists, and therapists for maximal recovery. Most recovery occurs within 6 months to a year after injury but can still happen several years later.
Resources
Glossary
Artery— blood vessel that delivers oxygen-rich blood from the heart to your tissues
Catheter—thin, hollow and flexible tube
Neuron—fundamental cell of the nervous system that receive and transmit electrical and chemical signals
Paraplegia—loss of motor and/or sensory function in the lower body parts
Spasticity—condition of increased muscle tone and involuntary muscle spasms
Tetraplegia—also known as quadriplegia, is the loss of motor and/or sensory function in the upper and lower body parts
Contributors: Gina Watanabe BS
References
- McDonald JW, Sadowsky C. Spinal-cord injury. The Lancet. 2002;359(9304):417-425. doi:10.1016/S0140-6736(02)07603-1
- Sekhon LHS, Fehlings MG. Epidemiology, Demographics, and Pathophysiology of Acute Spinal Cord Injury. Spine. 2001;26(24S):S2.