Cancer and Meningioma
- What Are the Grades of a Meningioma? Is Meningioma a Type of Cancer?
- What Is the Average Size of a Meningioma?
- Are Meningiomas Usually Life-Threatening?
- Is Meningioma Curable? What Happens If a Meningioma Is Left Untreated, and When Should a Meningioma Be Removed?
- Grade I Meningioma Treatment, Life Expectancy, and Recurrence
- Is Grade II Meningioma Serious, Can It Turn Cancerous, and What Is the Life Expectancy?
- Conclusions
- Key Takeaways
Meningiomas are the most frequent primary central nervous system (brain and spinal cord) tumors. They originate from the membranes (meningeal layers) that surround and protect the brain and spinal cord. Most of them arise sporadically, but certain predisposing factors such as family history, genetic diseases, radiation exposure, and hormonal therapy increase their occurrence.
They are classified into three grades according to the World Health Organization (WHO). Even though most of them are benign, their variable location can cause health implications. The symptoms a patient experiences depend on the tumor’s size and location. Some patients can be asymptomatic, while others can experience neurological problems. Diagnosis is made with clinical imaging. Magnetic resonance imaging (MRI) is the gold standard technique.
Their management is patient-centered; it is determined by a balance between the characteristics of the patient and the symptoms as well as the tumor size, mass effect and location on the brain. The benefits of surgery versus risks of treatment should be balanced for the final treatment plan.
What Are the Grades of a Meningioma? Is Meningioma a Type of Cancer?
The specific cellular features of a meningioma as analyzed by a pathologist under the microscope determine the tumor’s grade. The essential factor that defines the grade and the likelihood of recurrence after surgery is the rate at which the cells are growing within the mass. Fast-growing tumors are given a higher grade. Meningiomas are classified into 1 of 3 grades. For detailed grading information, please refer to the Meningioma Grading article.
Grade I meningiomas are slow-growing tumors with the lowest likelihood of recurrence after surgery. Notably, the majority (i.e., 80 to 81%) of meningiomas belong to this grade; they are benign (i.e., not cancerous), which means they do not typically invade adjacent tissues. Grade II are tumors that grow faster and are often called atypical meningiomas. They can invade adjacent structures, which makes them more challenging to treat and they tend to recur. Grade III meningiomas have the highest likelihood of recurrence. Grade III tumors are aggressive tumors (cancerous) that grow and spread more quickly. Often, they are called anaplastic or malignant meningiomas.
What Is the Average Size of a Meningioma?
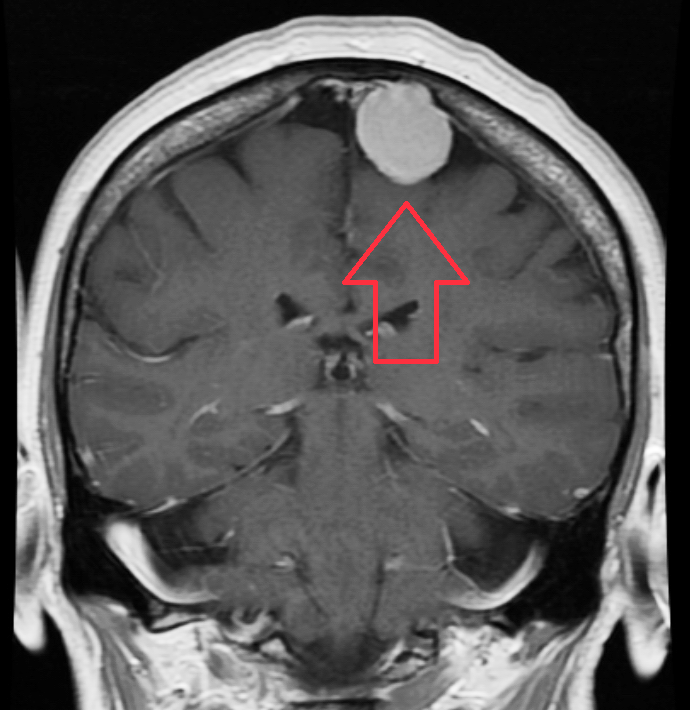
The size of a meningioma is variable and depends on the time of its diagnosis and the behavior of its cells or their growth rate (Figure 1). Several studies have shown that the growth rate of asymptomatic meningiomas is between 2-4 mm per year. On average, they measure around 3 cm at the time of diagnosis. Still, the range of size is broad and difficult to predict.
The size of the tumor alone does not determine the need for surgery. The combined factors such as the tumor’s size, location, presence of brain edema (swelling) and importantly the related symptoms dictate the need for observation versus surgical resection.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,000+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
Are Meningiomas Usually Life-Threatening?
Even though most meningiomas are benign and do not require immediate treatment, some can invade or compress essential brain structures and vital nerves, making them life-threatening if not treated. Factors such as the location, growth rate, and brain invasive capability are directly associated with their risk of being or becoming life-threatening.
Is Meningioma Curable? What Happens If a Meningioma Is Left Untreated, and When Should a Meningioma Be Removed?
In general, some types of meningiomas are curable. They can be managed with either observation, surgery, radiation therapy (radiosurgery), or a combination of these. Surgery offers the only chance for cure. Close observation can be an option for many patients with asymptomatic small-sized tumors. These lesions should be followed annually or biennially with serial imaging, most commonly with an MRI.
The main factors that determine the need for surgery and the optimal treatment modality are symptoms, tumor size and location, presence of brain swelling by the tumor, age, and the extent of medical comorbidities (if the patient is fit to safely undergo surgery). Meningiomas of higher grades can be challenging to treat, and survival rates are lower. In the cases where the tumor is growing or causing symptoms, the suggested standard of care is maximal safe surgical resection.
However, the ability to achieve complete surgical removal is determined by the factors mentioned previously and the invasion of nearby brain structures. After considering all the features of the patient, the decision on the best way to proceed is made. It should be emphasized that the management is patient-specific.
Grade I Meningioma Treatment, Life Expectancy, and Recurrence
Grade I tumors are the most common and represent more than 80% of meningiomas. They are low-grade which means they are relatively benign and grow slowly. Before deciding the treatment approach, the critical factors to consider are the patient presentation (i.e., symptoms, age, comorbid diseases), the tumor location in relation to the essential brain structures, and the expected tumor’s cellular architecture/growth rate. The approach is determined by balancing the risks of neurologic change from the treatment and the success of definitive therapy in controlling the tumor.
Upon reviewing the tumor characteristics, the initial management strategy for these tumors can be either observation with serial imaging, surgery, radiation therapy, or a combination of these. A multidisciplinary team is best suited to define the best possible route of therapy.
Although the life expectancy of patients suffering from these tumors is favorable, with an overall ten-year survival rate of more than 80%, patients should know that the treatment results vary according to the location of the tumor and the therapeutic approach. Finally, in cases where surgical treatment is performed, the recurrence rate is low (i.e., between 7 to 25%) when complete resection is achieved; however, this rate can rise in cases where the tumor cell structure shows potentially more aggressive features.
Is Grade II Meningioma Serious, Can It Turn Cancerous, and What Is the Life Expectancy?
Grade 2 meningiomas grow more quickly and have a higher percentage (i.e., 15-20%) of atypical tumor cells, which means they do not appear normal. The atypical characteristic of their cells makes them capable of transforming into cancerous lesions that can invade adjacent tissues. In addition, grade 2 meningiomas have an increased chance of growing back after surgically removed.
The recurrence rate at five years is 50%, with a 10-year overall survival rate of 53%. However, the presence of aggressive tumor cell morphology, large tumor size, and the presence of tumor in specific locations are the most common reported risks factors for a worse outcome after treatment. Finally, as is the case in lower grade meningiomas, the patient’s quality of life can be impacted by the tumor and the selected treatment modality.
Conclusions
Meningiomas represent around one-third of the primary tumors of the central nervous system. In most cases, the etiology is unknown, but there are specific predisposing factors that increase their occurrence. The majority of them are benign and asymptomatic, discovered incidentally. However, larger lesions can present with a wide variety of symptoms depending upon their location and size.
They are classified into three grades according to their structural characteristics. Observation, surgery, and radiation are the primary treatment modalities. A multidisciplinary healthcare team of neurosurgeons, oncologists and radiation specialists can optimize patient outcomes.
Key Takeaways
- Meningiomas are tumors that develop in the meningeal layers that surround and protect the brain and spinal cord. Their cause is not well understood but can be related to genetic and environmental factors.
- They are graded from 1 to 3, primarily according to their growth rate. Grade I tumors are the most common; they are benign and have the best prognosis. Grades II and III are serially more aggressive tumors that grow rapidly and can invade adjacent tissues.
- Symptoms can appear due to the tumor size and compression of the brain and spinal cord structures. Diagnosis is made based on clinical imaging modalities.
- Management involves close observation, surgery, and/or radiation therapy.