Transsphenoidal Surgery: What the Patient Needs to Know
- What Is Transsphenoidal Surgery?
- Who Performs Transsphenoidal Surgery?
- What Happens Before Transsphenoidal Surgery?
- What Happens During Transsphenoidal Surgery?
- What Happens After Transsphenoidal Surgery?
- What Are the Possible Complications of Transsphenoidal Surgery?
- What Is the Recovery Outlook After Transsphenoidal Surgery?
- Glossary
Overview
Transsphenoidal surgery is a procedure that involves accessing the base of the skull through the nose, usually to remove a tumor of or near the pituitary gland. The surgeon passes instruments through the nose and cuts the bone underneath the brain to reach the tumor. After removal of the tumor, the bone is replaced with a piece of fat from the abdomen or lining of the nasal mucosa and/or a bone graft from the nasal septum. Recently, more complex brain tumors, besides pituitary tumors, have been removed via the transsphenoidal route.
This procedure is less invasive than a craniotomy, it leaves no visible scar, and it allows for faster recovery. Most patients with vision problems due to the tumor before surgery experience vision improvement after surgery. However, successful treatment depends on the size of the tumor, the amount of area it covers, and how difficult it is to remove.
Complications specific to transsphenoidal surgery include damage to the pituitary gland and optic chiasm resulting in hormone deficiencies and new or worsening vision problems. Cerebrospinal fluid (CSF) leakage out of the nose or into the throat, meningitis, and stroke can also occur.
What Is Transsphenoidal Surgery?
Transsphenoidal surgery is a procedure that involves accessing the base of the skull through the nose. This is commonly done for the removal of tumors of or near the pituitary gland. The pituitary gland is a bean-sized structure that is critical for hormone release. It is located in a bony cavity of the sphenoid bone at the base of the brain behind the eyes.
Instead of performing a craniotomy, the surgeon passes instruments through the nose and drills the sphenoid bone underneath the brain at the level of the skull base to reach the tumor. This is a less invasive procedure that leaves no visible scar and allows for faster recovery.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,000+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
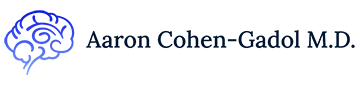
Figure 1. Removal of bone through the nasal passages (left) en route to a tumor at the base of the brain (right).
Transsphenoidal surgery can be performed with a microscope or, more recently, with an endoscope. During the endoscopic technique, a long thin instrument with a tiny camera and light at its end (endoscope) is inserted into a smaller opening in the nose and is more minimally invasive than traditional surgery.
Transsphenoidal surgery is commonly performed for tumors at or near the pituitary gland, including pituitary adenomas, Rathke cleft cysts, and selected meningiomas, craniopharyngiomas, and clival chordomas. Recently, more complex brain tumors have been removed via the transsphenoidal route.
Who Performs Transsphenoidal Surgery?
Transsphenoidal surgery is performed by a team of surgeons including a neurosurgeon and an ear, nose, and throat (ENT) surgeon (rhinologist) with specialized training in using the endoscope.
What Happens Before Transsphenoidal Surgery?
Before transsphenoidal surgery, a thorough pituitary hormone evaluation will be conducted, along with blood tests to check levels of hormones such as prolactin, cortisol, and thyroxine. In the case of prolactin-secreting tumors, pharmacologic treatment without surgery might suffice. If surgery is chosen, the surgeon will explain what the procedure will entail and its risks and benefits. You will fill out consent forms and other paperwork to inform the surgeon of relevant medical history, such as allergies, other medications you are taking, reactions to anesthesia, and any previous surgeries.
One week before surgery, nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (for example, Advil, Motrin), naproxen (for example, Aleve), and other prescribed NSAIDs, as well as blood thinners such as warfarin (for example, Jantoven, Coumadin), acetylsalicylic acid (for example, aspirin), and clopidogrel (for example, Plavix) should be stopped to decrease the risk of bleeding. This is not an all-inclusive list. Inform your physician of all medications and supplements you are taking, and follow his or her recommendations.
On the night before or morning of the surgery, your physician might ask that you not eat or drink anything (fasting) to prevent vomiting while under general anesthesia. To reduce the possibility of infection at the site of incision, showering with antiseptic soap might be required.
What Happens During Transsphenoidal Surgery?
Transsphenoidal surgery can take 2 to 4 hours to perform, depending on the size of the tumor, the amount of area that it covers, and how difficult it is to remove.
Step 1: Patient Preparation
The patient is placed on the operating table and given general anesthesia. If image guidance is used, a skull clamp must be placed on the patient’s head for immobilization during the operation.
Figure 2. The patient is placed in a “sniffing” position with the neck slightly flexed on a horseshoe headrest.
Step 2: Nasal Passage Dissection
The operation begins with gentle dissection of the nasal septum using local anesthesia. Bony structures in the midline are removed as the instruments advance toward the sphenoid bone encasing the tumor.
Figure 3. A small incision is made in the mucosa (left), and surgical instruments advance deeper into the nasal passages toward the sphenoid bone (right).
Step 3: Opening the Sella and Tumor Removal
A piece of bone encasing the pituitary gland (sella) is removed to expose the thin covering of the brain (dura). The dura is cut to reach the tumor and pituitary gland. With long surgical instruments, the tumor is dissected and removed. If an endoscope is used, the tiny camera at its end can visualize any remaining bits of tumor. These remnants can be removed or later treated with radiation.
Figure 4. The bone of the sellar floor is removed. The dotted red lines indicate the path of the incisions in the dura to adequately expose and remove the tumor.
Step 4: Closure
A piece of fat is taken from the abdomen and gently packed within the sella to fill in the empty space now devoid of tumor. Bone graft from the nasal septum is used to fill the hole made in the sella. The bones are secured using biologic (fibrin) glue for a watertight seal that prevents leakage of CSF. Finally, the nostrils might be packed to place gentle pressure on the nasal septum to control bleeding.
In this video, Dr. Cohen describes the techniques for transsphenoidal surgical resection of large or giant pituitary adenomas.
For more information about the technical aspects of the surgery and extensive experience of Dr. Cohen, please refer to the video case on Large Pituitary Adenoma: Resection Principles in the Neurosurgical Atlas.
What Happens After Transsphenoidal Surgery?
After transsphenoidal surgery, you are monitored in the intensive care unit (ICU) or regular hospital ward. Patients with Cushing disease are observed in the ICU to monitor for symptoms of a low cortisol level, which can be life threatening if not addressed quickly. Antibiotics might be administered if nasal packing is present. High urine output might indicate a deficiency in antidiuretic hormone and inability to concentrate urine (diabetes insipidus), which would require further investigation with laboratory tests.
Right after surgery, your nose might feel stuffy (congested), making it difficult to breathe normally. You might have an easier time breathing through your mouth. Excessive accumulation of mucus can cause nasal crusts to form for several weeks to months after surgery. This will go away over time. The ENT surgeon can also spray the nose with local anesthesia and remove the crusts.
Blood-tinged nasal drainage, nausea, and headache can occur after surgery and resolve on their own or are managed with medications. You might experience a loss of smell for several weeks. A tumor that is removed on or near the pituitary gland can also take parts of the pituitary gland with it, which can lead to an underactive pituitary gland and hormone deficiencies. An endocrinologist will check if the pituitary gland is producing normal amounts of hormones after surgery. If not, hormone-replacement medications might be recommended. The hospital stay is usually only 1 to 2 days.
At home, you should follow the instructions provided by your surgeon. A follow-up appointment with your neurosurgeon might be made for 1 to 2 weeks after surgery. Several appointments with the ENT surgeon will also be made until your nasal cavities have healed. During recovery, you might have headaches, which can be resolved with acetaminophen (Tylenol). In general, avoid high-intensity activities and take pain medicine as directed. Discuss when you can return to work with your physician. If you have sleep apnea, do not use your continuous positive airway pressure (CPAP) machine until you receive surgeon approval.
Activities
- Avoid strenuous activity (for example, lifting heavy items)
- Avoid straining during bowel movements
- Avoid high-risk activities that require attention (for example, driving)
- Try to walk 5 to 10 minutes every few hours and increase this time as tolerated
- Limit coughing, but if you must cough or sneeze, do so with your mouth open
- Do not blow your nose, use straws, or bend over at the waist
- Do not smoke or use nicotine products (for example, vaping), which can delay healing
- Drink water and eat foods high in fiber (for example, beans, whole grains, nuts, berries) to resolve constipation caused by the narcotics used for pain control during or after surgery
- Discuss activities such as returning to work or air travel with your physician
Incision Care
- Shower as early as the day after surgery
- Avoid submerging incision sites in the nose and abdomen in water (for example, bath, pool), and avoid applying lotions on the area
Medications
- Take acetaminophen (Tylenol) for headaches and other pain medications as directed by your physician
- Do not take NSAIDs (for example, Advil, Aleve), blood thinners (for example, aspirin, Coumadin), or other supplements without surgeon approval
When to Call Your Doctor
- Fever or chills
- Clear fluid with a metallic taste dripping from your nose or down your throat
- Excessive thirst or urination
- Increased drowsiness, confusion, nausea, vomiting, or headache
- New or worsening vision problems
- Nose bleeds that do not stop
- Seizures
What Are the Possible Complications of Transsphenoidal Surgery?
Complications of transsphenoidal surgery are rare but can arise due to damage to the pituitary gland or nearby structures. Damage to the normal pituitary gland can lead to hormone deficiencies and require hormone-replacement medications. Insufficient production of the antidiuretic hormone due to damage to the back of the pituitary gland (posterior lobe) causes frequent urination and excessive thirst (diabetes insipidus).
The optic nerves cross immediately above the pituitary gland, and damage to them can cause vision loss or worsening vision problems. CSF surrounding the brain can leak through the incision site of the dura and out through the nose, which might require surgery to fix and patch the area of the leak. Infection of the outer covering of the brain (meningitis), nasal deformities due to bone removal, bleeding, and stroke could also occur.
What Is the Recovery Outlook After Transsphenoidal Surgery?
Transsphenoidal surgery is a minimally invasive procedure for successfully removing a tumor, depending on its size and invasiveness. Smaller tumors that do not invade surrounding structures result in the best surgical outcome. The overall rate of surgical treatment success has been reported in ~70% of hormone-secreting pituitary adenomas. Improvement or normalization of vision problems due to the tumor can be observed in as high as 92% of patients.
Glossary
Cerebrospinal fluid—clear fluid that surrounds the brain and spinal cord
Craniotomy—procedure that removes a piece of bone from the skull to expose the brain; the bone is immediately reattached to its original location after surgery
Diabetes insipidus—a salt and water retention abnormality that leads to excessive urination and thirst caused by problems with antidiuretic hormone
Dura mater—outermost covering of the brain
Image-guided surgery—surgery using the patient’s computed tomography (CT) or magnetic resonance imaging (MRI) scans to guide the surgeon during the operation
Optic chiasm—an X-shaped structure formed by the 2 optic nerves crossing over each other
Sella or sella turcica—a saddle-shaped depression in the sphenoid bone where the pituitary gland resides
Seizure—a sudden burst of abnormal electrical activity in the brain that leads to uncontrollable spasms, twitching, or jerking
Contributor: Gina Watanabe BS
References
Mortini P, Losa M, Barzaghi R, et al. Results of transsphenoidal surgery in a large series of patients with pituitary adenoma. Neurosurgery 2005;56:1222–1233; discussion 1233. doi.org/10.1227/01.neu.0000159647.64275.9d