Surgery for Pituitary Tumors
The pituitary gland is a critical structure often known as the “master gland” because it produces hormones that regulate the functions of many organs throughout the body and ensures proper hormonal balance for everyday life. Weighing in at a mere 0.6 g, the pituitary gland is a small pea-sized structure located in a deep bony cavity behind the nose.
Tumors arising from the pituitary gland are almost always benign. However, due to the hormonal function of the gland and proximity to vital structures, pituitary tumors can overproduce hormones or compress other structures. This can cause a wide variety of symptoms.
Despite the evolving management options with drugs and radiation, surgery remains the treatment of choice in most cases and can be very effective. Regardless of the surgical approach, all neurosurgeons strive to maximize tumor resection, preserve vital structures, and optimize functional outcomes.
Historical Overview of the Surgical Approach
Pituitary surgery began in the late 18th century and was a challenging procedure that involved temporarily removing a large piece of skull bone from the top of the head (craniotomy) to access the pituitary gland. It took several years, pioneers, and approaches to consider using the intranasal corridor (transsphenoidal surgery through the nose) to reach the deep location of the pituitary gland through minimally invasive routes with less risk to the patient.
With the introduction of the operative microscope, accessing the pituitary gland through the nose via what is called the transsphenoidal technique gained popularity due to its ability to remove small pituitary tumors without damaging the surrounding tissues. The transsphenoidal approach is now commonly used, sometimes with the assistance of a long and thin instrument with a light and camera called an endoscope to assist with visualization of these small structures.
Indications for Surgery
Surgery is the first line of treatment for most pituitary tumors. In general, the goals of surgery are relief of tumor pressure on surrounding structures (mass effect), normalization of pituitary function and hormone production, reduction of tumor size, and collection of tumor samples for tissue analyses. Surgery may be indicated for tumors that:
- Compress adjacent structures, especially when vision is affected.
- Produce an excessive amount of hormone that is not controlled with medications.
- Overgrow their blood supply, which causes them to bleed (pituitary apoplexy). This is often considered an emergency.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,000+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
Surgical Management Options
There are two main surgical approaches to treating pituitary tumors. The transsphenoidal approach, when long instruments are passed through the nose, is the most commonly used technique because it is effective, minimally invasive, leaves no visible scar, and allows for faster recovery.
The transcranial approach involves creating a small opening in the skull temporarily (craniotomy) to reach the pituitary gland and is less often used but offers advantages when the tumor is large. A combination of both techniques is also a possibility in rare cases.
Preparation for Surgery
A comprehensive preoperative medical evaluation of the patient is undertaken, which may involve laboratory and imaging tests to determine if a patient is able to tolerate the surgery and recover appropriately. Surgeries are planned in detail to avoid complications and achieve the best possible outcomes. Surgeons will evaluate brain images taken preoperatively to determine the best surgical approach.
Additional images may be required in certain cases. Most of the preparatory planning may occur behind the scenes while the patient is waiting for the day of the operation. Patients can assist the healthcare team by attending their appointments and following the instructions provided. Specific instructions on how to prepare for surgery may be given as the day of the operation nears and includes fasting the night before the procedure.
The patient also meets the rhinology/otolaryngology (ENT) surgical team before the operation. The ENT surgeon will assist the neurosurgeon with the approach through the nose during the surgery via the use of the endoscope.
Transnasal Transsphenoidal Approach
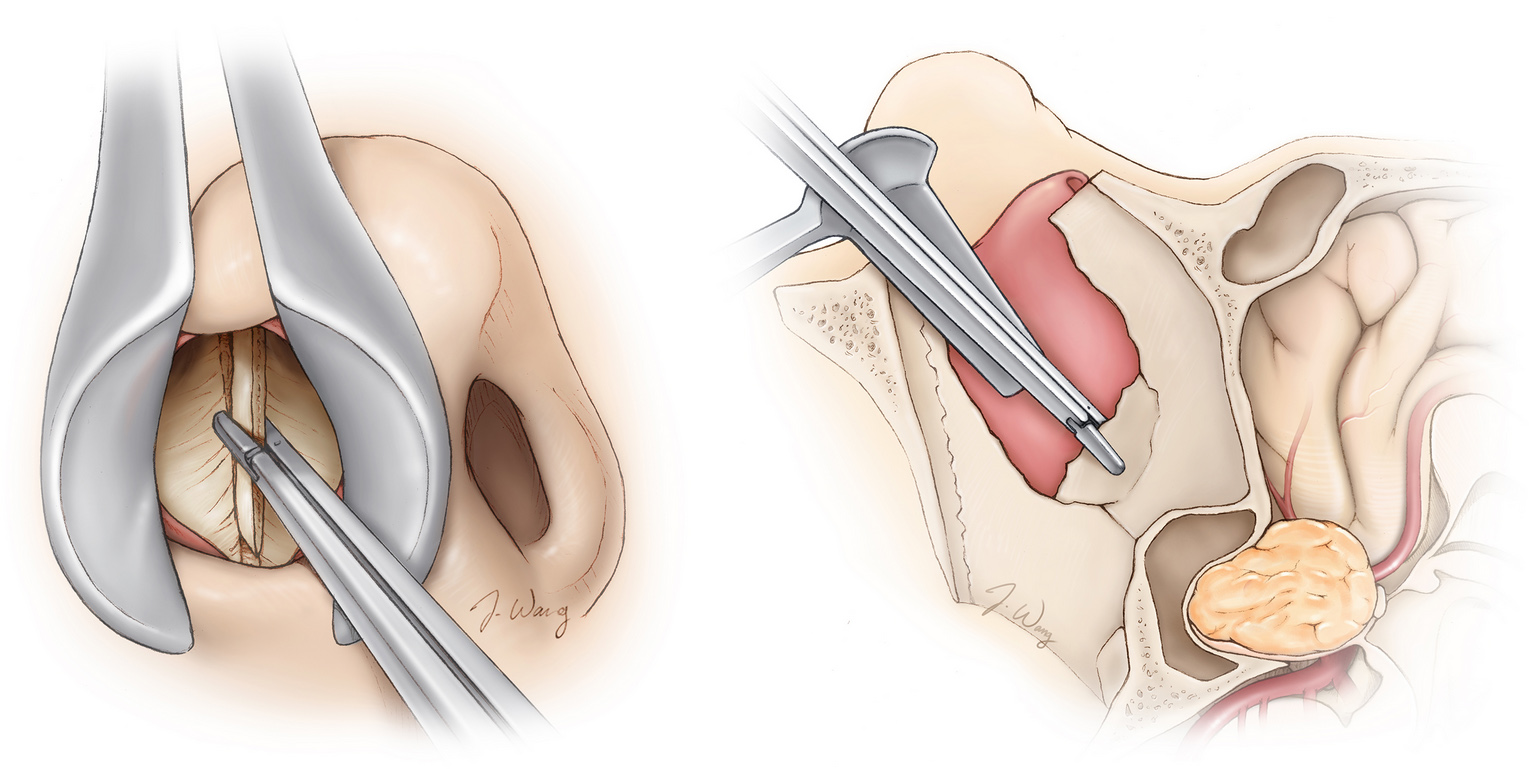
In the transnasal (through the nose) transsphenoidal approach (Figure 2), the pituitary tumor is reached by inserting long surgical instruments into the nose. The transsphenoidal approach can be performed in two ways. One involves using an operating microscope, and the other is performed with an endoscopic camera.
A combination of both is also possible. When a traditional microscope is used, surgeons can directly visualize the operating area and remove the tumor. In the endoscopic approach, a tiny camera is inserted through a small incision, producing less tissue disruption. This technique offers a wider view. The route and equipment used are specific to the characteristics of the patient and the tumor and may be influenced by the surgeon’s preference and training.
When the patient arrives at the operating room, general anesthesia is given, the patient is positioned on the operating table, and the nose is cleaned and prepared for access. Specific image guiding equipment may be set up and positioned. The site of access is incised, and the microscope or endoscope is inserted through the nose.
At the back of the nose, the sphenoid bone is visualized and carefully removed to enter the skull. Immediately behind the sphenoid bone, a thick protective layer of tissue called the dura is encountered and cut. At this stage, the tumor and pituitary gland are visualized. The tumor is removed in pieces while its surroundings are carefully preserved. The goal is to remove the tumor entirely, but if the risk of damaging adjacent structures is high, some tumor tissue can be left behind and later monitored and treated with radiation therapy if sign of growth on imaging is noted.
Once tumor resection is achieved, the surgeon ensures that there is no active bleeding and closes each layer. The bone is replaced with a piece of fat from the abdomen or lining of the nasal mucosa, and/or a bone graft from the nasal septum.
Transcranial Approach
The transcranial approach is exceedingly rarely used (Figure 3). It is favored when pituitary tumors are large and/or have a complex growth pattern. The major advantage of this approach is the improved operative visibility of the tumor and its extension to adjacent structures. However, an important limitation of this approach is that it becomes difficult to see and access the part of the tumor within the bony cavity called the sella turcica.
This part of the tumor is what would be directly visualized using the transsphenoidal approach. If there is a significant portion of tumor that cannot be accessed in this bony cavity, the transsphenoidal approach may also be used at a later stage.
The initial preparation during surgery is similar to that of transsphenoidal surgery. The patient first receives general anesthesia. Once asleep, the patient is positioned on the operating table, and the scalp skin behind the hairline is cleaned and prepared. The forehead or the side of the head are the most commonly used access locations, and a small area of hair may be shaved off. The superficial skin and muscles are incised before removing a piece of the skull (craniotomy).
Before reaching the brain, the protective membranous covering called the dura is cut and reflected. Once the brain is exposed, it is gently elevated to create a safe path to the pituitary gland. The tumor is located and removed carefully away from the surrounding structures. After tumor removal, the surgeon ensures that there is no active bleeding. The closure is done by layers with replacement of the original bone flap. Finally, the muscle and scalp are approximated and fixed with sutures.
Postoperative Care
Once the surgery is complete, the patient is taken to the recovery room, where vital signs are monitored as the patient awakens from anesthesia. Depending on the operation, patients can be taken to a regular room or the intensive care unit for observation and monitoring. In both operative approaches, nausea and headache can be present. Nasal congestion is common in the transnasal transsphenoidal approach.
A multidisciplinary team is involved in the patient’s care to control symptoms and ensure adequate hormonal levels. One or two days following the procedure, an imaging exam is performed. If everything goes well and the patient is stable, hospital discharge with instructions is the final step.
The endocrinology team plays a critical role in the care of patients during the postoperative period.
Surgical Risks
As with all procedures, risks are present. General complications include bleeding, infection, adverse reactions to anesthesia and/or medications. Some complications specific to pituitary surgery include vision loss, damage to the normal functioning pituitary gland, hormonal alterations, cerebrospinal fluid leakage through the nose, meningitis, and nasal deformity and/or bleeding.
Outcomes
The success of surgery depends on the amount of tumor removed during the procedure and preservation of surrounding healthy structures. Detailed imaging evaluation before the surgery is critical to locate tumor extension and determine the optimal surgical approach. Many patients who initially present with visual alterations experience an improvement following surgery.
However, visual deterioration can still occur in a small number of patients. Hormone production of the pituitary gland depends on its preoperative function. In some cases, hormonal function returns to normal, while in others, it fails to return to baseline. Hormone replacement therapy can be used when needed. Tumor recurrence can occur depending on the type of tumor and the amount of tumor removed during surgery, so regular followup is often advised.
In summary, pituitary tumors can be associated with severe hormonal and visual alterations. The surgical management of these lesions involves a multidisciplinary team that cares for the patients before, during, and after the procedure. More commonly, the transnasal transsphenoidal approach is selected. However, the transcranial approach is always a valuable option, especially for large tumors with complex growth patterns.
The treatment goals are the re-establishment of normal pituitary and neurologic function, elimination of mass effect, minimization of tumor recurrence, and, in specific cases, definitive tumor diagnosis. The surgical approach requires a balance between treatment risks and patient benefits.
Key Takeaways
- In most pituitary tumor cases, surgery remains the treatment of choice. Transnasal transsphenoidal surgery is a minimally invasive technique that is most commonly selected.
- Medical and hormonal management are fundamental before, during, and after the procedure. Surgical planning via imaging optimizes tumor resection.
- Complications of pituitary surgery include vision loss, hormonal alterations, infections, leak of cerebrospinal fluid, and nasal deformity.
- Surgical success depends on the tumor size, extent of removal, and preservation of surrounding healthy structures.