What is ETT Surgery?


Endoscopic transnasal transsphenoidal surgery (ETTS) can be a lot to remember. Fortunately, it goes by several other names.
“Endoscopic endonasal approach”, or “EEA” for short, is perhaps the easiest one to remember. “Endoscopic” refers to the use of a special camera called an endoscope.
“Endonasal” combines “endo”, meaning “within”, and “nasal”, referring to the nose, to describe a procedure performed through the nasal passages.
EEA is thus a minimally invasive way to perform brain surgery. Instead of a traditional craniotomy involving an incision on the scalp, an EEA allows a surgeon to access the brain in a way that hastens recovery and leaves no visible scar.
But not all brain tumors can be accessed in this way. EEA is typically reserved for tumors at the base of the skull. This can include pituitary tumors, meningiomas, craniopharyngiomas, cystic lesions such as Rathke’s cleft cysts, and chordomas, among others.
What Is Transsphenoidal Surgery?
Transsphenoidal surgery is another term for EEA that combines “trans”, meaning “across” or “through,” and “sphenoidal”, relating to the sphenoid bone at the base of the skull. During an EEA, the sphenoid bone is encountered and parts of it are removed to access the brain.

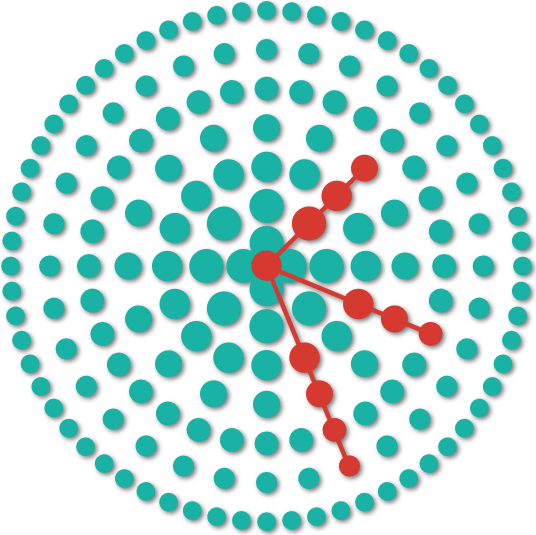
Figure 1: An EEA is demonstrated. Long instruments are inserted into the nasal passages en route to a tumor at the skull base.
During this process, you are typically unconscious under general anesthesia. To start, a slender, long instrument equipped with a miniature camera and illumination source, collectively termed the “endoscope,” is introduced through one of the nasal orifices.
This surgery is most often performed by a team consisting of a neurosurgeon and an otorhinolaryngologist (or ear, nose, and throat surgeon) who work together to expose and ultimately remove the tumor.
As the surgeons use their instruments under endoscopic guidance to progress towards the sphenoid bone (which envelops the tumor and must be penetrated), bony and cartilaginous structures along the midline are removed.
Parts of the sphenoid bone are carefully removed to expose the brain’s tough membranous covering (dura). The dura is incised to expose the brain. The pituitary gland (and its tumor) are the most prominent parts of the brain in view.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,500+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.

Figure 2: Parts of the sphenoid bone are removed with the grey dura lying underneath. The dotted marks represent the planned incision lines.
Once exposed, the neurosurgeon will complete the removal of the tumor by dissecting it away from normal surrounding tissue with the goal of leaving normal pituitary tissue intact. This procedure is a relatively short brain tumor surgery and typically takes 2 to 4 hours to complete.
While any type of brain surgery is considered major or serious due to the risk of injuring important nearby structures, the relatively short procedure time and minimally invasive nature of the EEA allows for a quicker recovery time than other more traditional types of brain surgery.
How Successful Is Transsphenoidal Surgery?
Pituitary tumor surgery is often successful. For individuals with hormone-secreting pituitary adenomas, the reported success rate of surgical treatment is approximately 70%. Furthermore, approximately 90% of patients experience an improvement or full restoration of visual deficits caused by the tumor after the procedure.
However, it is important to acknowledge that the success rate of transsphenoidal surgery can vary based on multiple factors, including the tumor's pathologic subtype, size, invasiveness, the expertise of the surgical team, as well as the individual patient's overall health.
In terms of survival rate, patients affected with pituitary gland tumors often have a positive prognosis, with most patients having normal lifespans, especially when the tumor is benign and effectively treated.
What Happens After a Pituitary Tumor Is Removed?
Following transsphenoidal surgery, you will be monitored in the intensive care unit (ICU) or a standard hospital ward. Immediately after the procedure, your nares may be filled with nasal packing, or you may experience nasal congestion.
This can make regular breathing somewhat challenging. Breathing through your mouth can offer improved comfort during this period.
Some nasal drainage containing a slight red tinge is normal after the procedure. However, persistent watery drainage, or drainage that is strictly red (bloody), should be reported to a member of your care team.
This may represent a cerebrospinal fluid leak or active bleeding, which should be urgently addressed before discharge.
During the recovery period, it is not unusual to experience pain, occasional bouts of nausea, or headaches, all of which typically resolve without intervention. If needed, headaches and pains can be managed with prescribed medications.
Nausea and vomiting are relatively common side effects of the anesthetic agents administered during surgery and can be managed with anti-nausea medications.
Besides ensuring that your pain and nausea are under control, the medical team will also perform blood tests to monitor for any electrolyte imbalances and correct any as needed.
In preparation for hospital discharge, they will also coordinate the date and time of your first follow-up appointment, or provide you with instructions for doing so.
Attending all follow-up appointments are important because a pituitary tumor can potentially come back, or recur, after surgery. Serial imaging tests can help to determine if the pituitary tumor is growing and prompt next steps for treatment.
What Can You Not Do After Pituitary Surgery?
After pituitary surgery, avoiding strenuous physical activities such as heavy lifting (or any activity involving straining) for several weeks is essential to minimize the risk of complications such as cerebrospinal fluid leakage.
Activities involving “straining” are relatively common in daily life and will require conscious effort to avoid. This can include blowing your nose forcefully and “bearing down” during bowel movements. Stool softeners or laxatives may be prescribed to reduce these episodes.
Will I Lose Weight After a Pituitary Tumor Is Removed?
The impact on weight after the removal of a pituitary tumor can vary depending on several factors. Pituitary tumors can affect hormonal regulation and balance with the body, and their removal may lead to changes in metabolism.
In some cases, normalizing hormone levels, especially if the tumor was causing excessive growth hormone or cortisol production, can result in weight loss over time. However, the extent of weight loss and the timeline for such changes can differ from person to person.
Not all individuals will experience significant weight loss after pituitary tumor removal, and other factors, such as diet and exercise, can play a more crucial role in managing body weight. Discussing your specific case with your healthcare provider will help tailor the approach based on your medical history and is essential to optimal, healthy weight loss.
Key Takeaways
- Endoscopic endonasal transsphenoidal surgery is a minimally invasive procedure to access the brain through the nasal passages.
- Success rates for transsphenoidal surgery can vary depending on different factors but are generally favorable.
- After pituitary tumor removal, patients may experience nasal congestion, minor bleeding, or nausea, which can be managed with appropriate medications provided by your healthcare team
- Avoid heavy lifting and other activities involving straining for several weeks after the procedure.
- Weight loss after pituitary tumor removal may occur due to hormonal changes, but the extent and timing of such loss varies considerably among individuals.