Endoscopic Transnasal Transsphenoidal Surgery
Endoscopic Transnasal Transsphenoidal Surgery (ETTS) is a minimally invasive surgical technique primarily used for treating tumors within the pituitary gland. This procedure has revolutionized the approach to pituitary tumor surgery, offering numerous benefits over traditional methods. This article delves into ETTS, exploring its benefits, risks, and recovery process.
What Is Endoscopic Transnasal Transsphenoidal Surgery?
ETTS is a specialized procedure designed to access and treat conditions in the pituitary gland by entering through the sphenoid sinus located behind the nasal passages. The surgery can be performed using an endoscope or a microscope to guide the surgeon, offering a minimally invasive approach with no visible scarring and a faster recovery time.
The pituitary gland, often referred to as the "master gland," is critical for hormone regulation in the body. Tumors in this gland can lead to hormonal imbalances and pressure on nearby structures, such as the optic nerves, causing vision problems. ETTS is primarily used to remove these tumors and restore normal function.
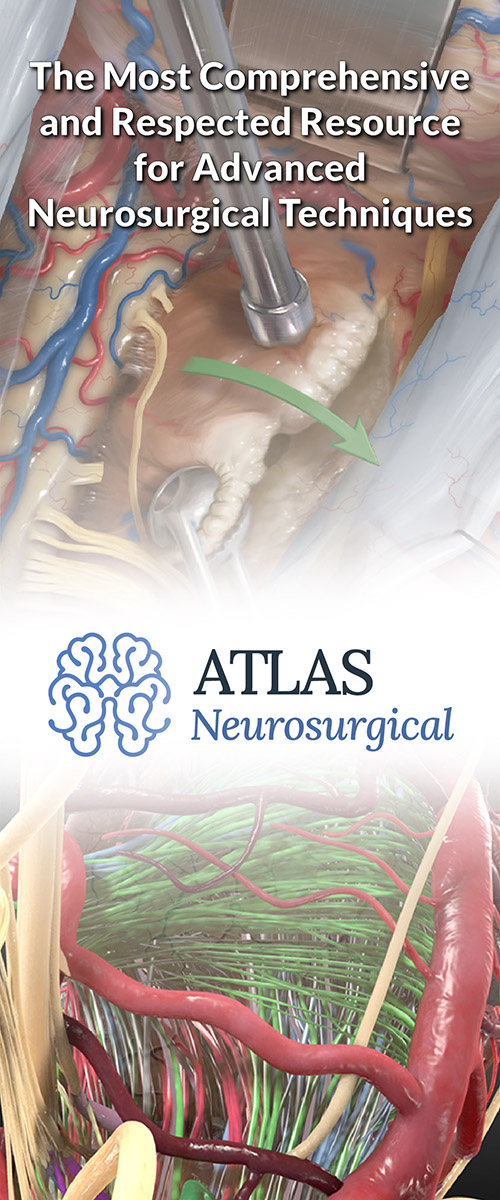
Figure 1: The illustration demonstrates the surgical approach and instrumentation to access a pituitary tumor within the sella.
What Are the Benefits of ETTS?
- Minimally Invasive: ETTS avoids large incisions and significant skull manipulation, reducing tissue disruption and trauma. This results in less postoperative pain and a quicker return to normal activities.
- Lower Risk of Complications: The reduced invasiveness of ETTS leads to a lower risk of complications such as infections, cerebrospinal fluid leakage, and damage to surrounding structures.
- Improved Hormonal and Vision Outcomes: For patients with hormone-secreting pituitary adenomas, ETTS often results in the improvement or normalization of hormone levels and vision problems. Approximately 70% of patients with hormone-secreting tumors experience successful outcomes, and vision issues improve in up to 92% of cases.
- Preservation of Healthy Tissue: ETTS allows for precise targeting of the tumor, minimizing damage to healthy tissue and structures.
- Cosmetic Benefits: Since the surgery is performed through the nasal passages, there are no visible external scars, preserving the patient's appearance.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,000+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
What Are the Risks and Complications?
Despite its benefits, ETTS carries certain risks and potential complications. Understanding these is crucial for informed decision-making.
- Postoperative Hypopituitarism: Approximately 19% of patients may experience hypopituitarism, a condition where the pituitary gland does not produce adequate hormones. This may require hormone replacement therapy.
- Diabetes Insipidus: Around 17% of patients may develop diabetes insipidus, characterized by frequent urination and excessive thirst due to insufficient antidiuretic hormone production.
- Sinus Problems: Temporary sinus congestion, discharge, or crusting is common post-surgery. These symptoms typically resolve as healing progresses.
- Headaches and Hormonal Imbalances: Some patients may experience headaches and hormonal imbalances, requiring monitoring and management.
- Cerebrospinal Fluid Leakage: Although rare, this complication may necessitate further intervention.
- Infection and Vision Problems: Infection at the surgical site and vision issues due to optic nerve damage are potential risks.
- Delayed Healing and Scar Tissue: Some patients may face delayed healing of the nasal passages and development of scar tissue, leading to recurrent symptoms.
What to Expect During and After Surgery?
During Surgery
ETTS is performed under general anesthesia. The surgeon inserts an endoscope through the nasal passages to access the sphenoid sinus and the pituitary gland. The surgery typically takes about 2 to 4 hours.
After Surgery
Following surgery, patients are taken to a recovery room, to awake from anesthesia. After this, postoperative care includes monitoring in the ICU or a regular hospital ward.
Patients may experience nasal congestion, blood-tinged nasal drainage, nausea, and headaches. Some patients also report a diminished ability to smell following ETTS, and may have complaint of a persistent unpleasant smell.
These symptoms usually resolve naturally or with medication. Hospital stays are generally short, often lasting only 1 to 2 days.
Recovery and Aftercare
Recovery from ETTS varies among individuals but generally involves a few key aspects:
- Nasal Care: Patients may experience nasal congestion and crusting for several weeks to months. Proper nasal care and avoiding actions like blowing the nose forcefully are crucial.
- Activity Restrictions: Avoiding strenuous activities, heavy lifting, and activities that increase intra-abdominal pressure is important to prevent complications such as cerebrospinal fluid leakage.
- Follow-Up Appointments: Regular follow-up appointments with the neurosurgeon and ENT specialists are essential to monitor healing and manage any complications.
- Medication Adherence: Following the prescribed medication regimen is critical for managing symptoms and ensuring a smooth recovery.
Long-Term Outlook and Success Rates
The success of ETTS largely depends on the tumor's size, type, and invasiveness, as well as the surgical team's expertise. Hormone-secreting pituitary adenomas have a surgical success rate of about 70%, with significant improvements in vision issues for 92% of patients. The 5-year survival rate for individuals with pituitary tumors is an impressive 97%.
Key Takeaways
- Endoscopic Transnasal Transsphenoidal Surgery offers a minimally invasive and effective solution for treating pituitary tumors.
- While it comes with certain risks, the benefits of improved hormonal and vision outcomes, lower complication rates, and faster recovery make it a preferred choice for many patients.
- Understanding the procedure, potential risks, and recovery process is vital for patients considering this surgery.
- With proper care and follow-up, ETTS can significantly improve quality of life and long-term health outcomes.