Treatment of Cushing's Disease
Cushing's disease is a hormone disorder caused by the presence of a benign brain tumor in the pituitary gland. This tumor produces excess adrenocorticotropic hormone (ACTH), which subsequently triggers the adrenal glands above the kidneys to generate an abundance of the "stress hormone" cortisol.
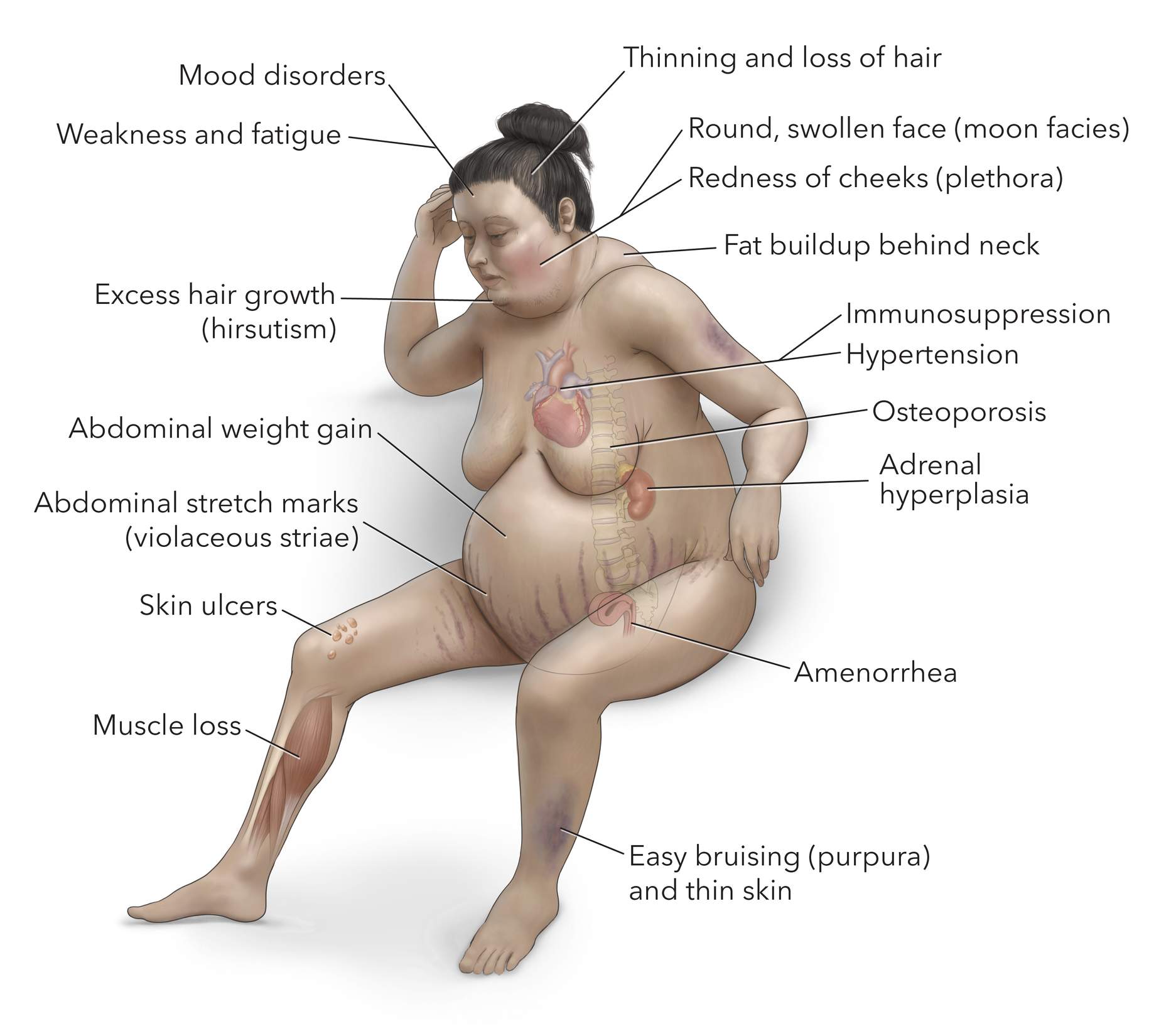
Surplus cortisol disturbs the body's regular operations, giving rise to an array of symptoms like weight gain, a rounded facial appearance ("moon face"), thin skin, muscle weakness, and shifts in mood. These symptoms wield considerable influence over both the physical and emotional well-being of an individual.
How fast Cushing's disease progresses can vary widely from person to person. It depends on several factors, including the size and nature of the pituitary tumor. The diagnosis of Cushing's disease entails a combination of clinical assessment, laboratory examinations, and imaging investigations.
The approach to treatment varies based on the gravity of the condition and might encompass surgical excision of the pituitary tumor, administration of medications to reduce cortisol levels, or the utilization of radiation therapy. In this article, we provide an overview
Medical Treatment of Cushing’s Disease
Various medications can be employed to medically manage Cushing's disease. These drugs function by either decreasing cortisol production or minimizing the impacts of cortisol within the body.
Pasireotide (Signifor): Pasireotide (Signifor) is an analogue of the somatostatin hormone. It operates similarly to somatostatin and effectively binds to ACTH-secreting tumors, thereby suppressing ACTH secretion.
It's worth noting that pasireotide might elevate blood sugar levels (hyperglycemia). Therefore, patients with diabetes mellitus require careful evaluation, and their existing diabetic treatments should be optimized before initiating pasireotide therapy.
Ketoconazole: Ketoconazole, an antifungal medication, has been utilized off-label to treat Cushing's disease. It serves as a cortisol synthesis inhibitor, capable of dampening cortisol production and addressing elevated cortisol levels.
However, ketoconazole should only be used under the supervision of an experienced endocrinologist, given its potential for notable side effects and interactions with other drugs. Common adverse effects include nausea, vomiting, abdominal discomfort, headaches, and alterations in liver function tests.
Osilodrostat (Isturisa): Osilodrostat (Isturisa) is a medication for Cushing's disease that belongs to the cortisol synthesis inhibitor class. It obstructs the enzyme 11-beta-hydroxylase, pivotal in cortisol production.
Some frequent side effects of osilodrostat include nausea, diarrhea, headaches, fatigue, and reduced appetite. FDA-approved in 2020, osilodrostat has exhibited promising outcomes in clinical trials for managing Cushing's disease.
Metyrapone (Metopirone): Metyrapone (Metopirone) is used in the medical management of Cushing's disease. Operating as a cortisol synthesis inhibitor, it blocks the enzyme 11-beta-hydroxylase involved in cortisol production.
Common side effects of metyrapone include gastrointestinal disruptions like nausea, vomiting, and abdominal pain, in addition to dizziness and fatigue.
Mifepristone (Korlym, Mifeprex): Mifepristone acts as a glucocorticoid receptor antagonist, counteracting the effects of cortisol. As a result, it alleviates symptoms linked to excessive cortisol levels in individuals with Cushing's syndrome or disease.
Like any medication, mifepristone could induce side effects, including nausea, fatigue, headaches, and fluctuations in hormone levels.
Surgical Treatment of Cushing’s Disease
At present, the only potentially curative treatment option for ACTH-secreting pituitary adenomas is pituitary surgery. This is typically performed through the nose (transnasal) with the use of a long special camera called an endoscope. This is an effective procedure that leads to symptom decrease or complete resolution in approximately 80% to 85% of patients.
The general steps are as follows. Upon entry into the operating room, general anesthesia is administered, and the patient is positioned on the surgical table. The nasal area is meticulously cleansed and prepared for access.
The surgical procedure entails creating an incision at the access point within the nose and introducing an endoscope through the nasal passage. With adept precision, the surgeon guides long instruments through the nasal cavity and gently drills into the sphenoid bone to reach the tumor.
Why should you have your surgery with Dr. Cohen?
Dr. Cohen
- 7,000+ specialized surgeries performed by your chosen surgeon
- More personalized care
- Extensive experience = higher success rate and quicker recovery times
Major Health Centers
- No control over choosing the surgeon caring for you
- One-size-fits-all care
- Less specialization
For more reasons, please click here.
The tumor is extracted in fragments, while critical surrounding structures are preserved. The primary aim is complete tumor excision; however, if there is a high risk of harming neighboring tissues, a portion of the tumor may be intentionally left behind.
After successful tumor removal, the surgeon ensures that bleeding is controlled and proceeds to close each layer. The transsphenoidal approach is less intrusive than a traditional craniotomy, leaves no scar, and facilitates a swifter recovery process.
Radiation Therapy for Cushing’s Disease
Radiation therapy is another treatment option for Cushing's disease. It may be used after surgery to inhibit growth from tumor remnants, or as primary treatment when surgery is not feasible.
Radiation therapy involves the precise application of high-energy radiation beams to specifically target and damage cells of the pituitary tumor (adenoma). The objective of this therapy is to restore normal hormone levels, alleviate symptoms, and prevent tumor growth.
Radiation therapy can be administered through a conventional fractionated approach or via stereotactic radiosurgery.
Traditional External-Beam Radiation: In the conventional approach of external-beam radiation therapy, a precisely focused radiation beam is directed at the tumor. Usually, this treatment is given five times a week for several weeks, and in some cases, it may extend over multiple years to effectively control tumor growth and hormone release.
Stereotactic Radiosurgery: Stereotactic radiosurgery involves the delivery of high-energy radiation beams in a single, extended session. Despite being named "radiosurgery" due to its exceptional accuracy, it does not involve an actual surgical incision.
The most common complication following radiation therapy for Cushing's disease is hypopituitarism, a condition where the pituitary gland fails to normally produce one or more hormones. Additionally, radiation therapy may cause damage to the nerves involved in vision, potentially leading to visual field cuts and blurry vision.
Headaches, fatigue, and changes in cognitive functioning may also occur, but are typically transient. Although the objective of radiation therapy is to precisely target the tumor, there is a chance of unintended harm to neighboring healthy tissues, leading to a condition known as radiation necrosis.
While this condition is rare, it can lead to delayed complications that surface months to years after treatment. Symptoms of radiation necrosis can include headaches, memory deterioration, personality changes, and seizures.
Observation for Cushing’s Disease
In certain instances of Cushing's disease where the condition is mild or asymptomatic, a strategy known as observation, or watchful waiting, might be employed. This approach involves vigilant monitoring of the patient's health and hormone levels.
The decision to pursue observation for a pituitary tumor is made with careful consideration. When a medical professional determines that the tumor is small and exerts minimal impact on a patient's daily life, observation can serve as a viable alternative to immediate intervention.
Your neurosurgeon or endocrinologist will likely establish a regular testing schedule to consistently assess the tumor's status and your overall condition over time. This often involves yearly MRI scans.
If the tumor exhibits no significant growth and causes minimal hormone excess and symptoms, surgery might not be necessary.
How Much Weight Can You Gain With Cushing’s Disease?
The degree of weight gain can differ among individuals, influenced by factors like disease severity and duration, individual metabolism, lifestyle, and underlying health conditions.
The weight gain may also be gradual, making it difficult to measure exactly how much weight gain can be attributed to Cushing's disease.
While effective treatment of Cushing's disease removes the source of abnormal weight gain, it will not lead to drastic weight loss overnight. Returning to your normal weight can still be challenging and require substantial effort.
Due to the cumulative impact of Cushing's disease on your body over a potentially long period of time, it may take months or even years to feel like yourself again. Celebrate every step forward in your health journey, seek support from family and friends, and remember to take care of both your mind and body
Key Takeaways
- Transsphenoidal surgery is the gold-standard treatment for Cushing's disease.
- Radiation therapy is an option for Cushing's disease in combination with surgery, or when surgery may not be feasible.
- Medications like ketoconazole, osilodrostat, mifepristone, and metyrapone can be used to lower cortisol levels.
- Observation is a viable option when the tumor is small and produces minimal to no symptoms or hormone changes.